The American healthcare system is undergoing a fundamental transformation in how medical services are delivered, measured, and reimbursed. For decades, fee-for-service models incentivized volume over value, rewarding providers for delivering more services regardless of outcomes. In this blog, we will discuss value-based care models that are gaining momentum across the healthcare landscape, promising better patient outcomes at lower costs through aligned incentives and coordinated delivery systems.
The Value-Based Paradigm Shift
Value-based care fundamentally represents a philosophical shift in defining healthcare success based on patient outcomes and the costs to provide those outcomes. Value-based care gained traction as a concept after the 2006 publication of “Redefining Health Care” by Harvard economist Michael Porter, who argued that competition in healthcare should be based on delivering value to patients rather than shifting costs, increasing bargaining power, or growing sites of service. More than a philosophy, value-based care entails various payment and delivery models that tie provider reimbursement to specific metrics of quality of care and cost containment rather than strictly volume of service.
Value-based care can include anything from simple pay-for-performance bonuses to complex global payment models, where providers accept financial responsibility for both quality and total costs of care for a defined population of patients. The Centers for Medicare and Medicaid Services (CMS) has driven some of this change through programs such as the Medicare Shared Savings Program for Accountable Care Organizations, which has over 11 million beneficiaries. Commercial insurers have had a parallel experience, and about 60% of healthcare payments are now being paid through a commercial contract with a value-based component, according to the Health Care Payment Learning and Action Network.
Restructuring Care Delivery for Value
Value-based care requires more than payment reform: It requires structural changes in the organization and delivery of healthcare. Models of integrated care that support coordination of services across care settings, replacing traditional siloed approaches, emerge from this shift. As examples of this need for collaboration, primary care practices will become medical homes that provide comprehensive care for patients, while hospitals will develop post-acute care networks to functionally and financially secure smooth transitions and limit readmission at further expense.
Clinical decision-making must also change within value-based frameworks. Protocols, which use evidence to specify best practices for patients with common chronic diseases, will require less variation in care preferences between providers. The Virginia Cardiac Services Quality Initiative tackled intra-provider variation by requiring standardized care pathways for cardiac surgery, reducing complications by 36% and reducing length of stay by 1.4 days among patients in participating hospitals. Success with value-based systems may well be defined by the degree of substantial resource shift toward prevention and early intervention.
Addressing Health Equity in Value-Based Models

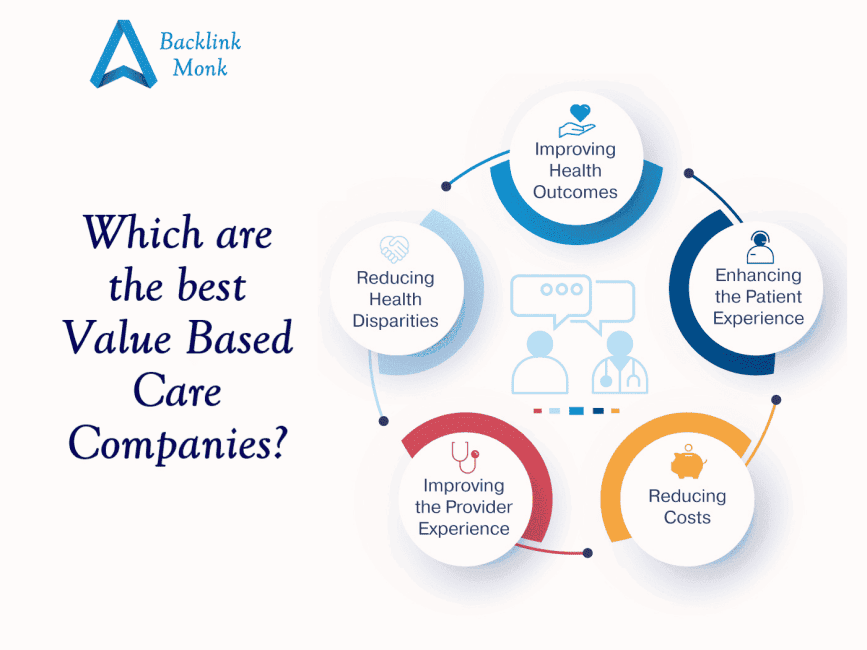
As value-based care continues to develop, more advocates are concentrating on ensuring these new programs actually promote health equity rather than exacerbate the inequities that already exist. Value-based care has often generated unintended consequences for disadvantaged populations, as providers serving those populations tended to underperform on quality metrics relative to their peers, often because their quality measures were not adequately risk-adjusted for issues related to social factors and structural barriers to care. More sophisticated approaches are now incorporating equity-focused design elements.
The Massachusetts Medicaid program was one of the first systems to implement risk adjustment to account for social risk factors, which allow increased payments for beneficiaries who have housing instability, food insecurity, and neighborhood deprivation. This is an innovative approach to paying for health care that means providers can continue to serve vulnerable populations, and the system can still hold them accountable for quality outcomes.
Some models are now even integrating explicit equity metrics into programs to accompany traditional quality measures. For example, the Accountable Health Communities Model will assess participants not only on overall performance, but also based on meeting the aims to decrease gaps between demographic groups.
Conclusion
Multi-payer collaboratives in states such as Colorado, and Delaware provide examples of how coordinated approaches can expedite changes in the delivery system. Patient engagement is another frontier. Most value-based change from providers has happened without meaningful consumer engagement in the design and implementation of patient-centered systems. Innovative models that promote involvement of patients as active participants in their care, such as patient-designed outcome measures, shared decision-making tools, or financial incentives, may positively impact value-based care.
Finally, digital health is likely to become further integrated into value-based delivery systems with virtual care, remote monitoring, and AI-based decision support providing standard aspects of care. These health technologies have the potential to expand provider capacity as well as to allow for continuous data to be available to support quality improvement and risk stratification. However, the challenge will be where, how, and when we implement technology so it adds to and does not detract from the human relationships that are valuable in care.

I extremely enjoyed the standard information an individual provide for your visitors?
Hey very nice web site!! Guy .. Excellent .. Amazing .. I will bookmark your website and take the feeds also?KI’m satisfied to seek out a lot of helpful info here in the put up, we’d like work out extra strategies on this regard, thank you for sharing. . . . . .